Migraine and Panic Attacks: How They Interact and What You Can Do
If you experience migraines, you know the debilitating pain, visual disturbances, and nausea they can bring. But did you know that migraines and panic attacks often occur together? It can be frightening to experience both, leaving you wondering if these conditions are connected and, more importantly, what you can do to find relief. This article will explore the intricate relationship between migraines and panic attacks, offering practical strategies to manage both. We will draw upon evidence-based information from reputable sources like the American Psychological Association (APA), the National Institute of Mental Health (NIMH), and the Mayo Clinic to provide you with a clear and supportive understanding of this complex interplay.
Understanding Migraines and Panic Attacks
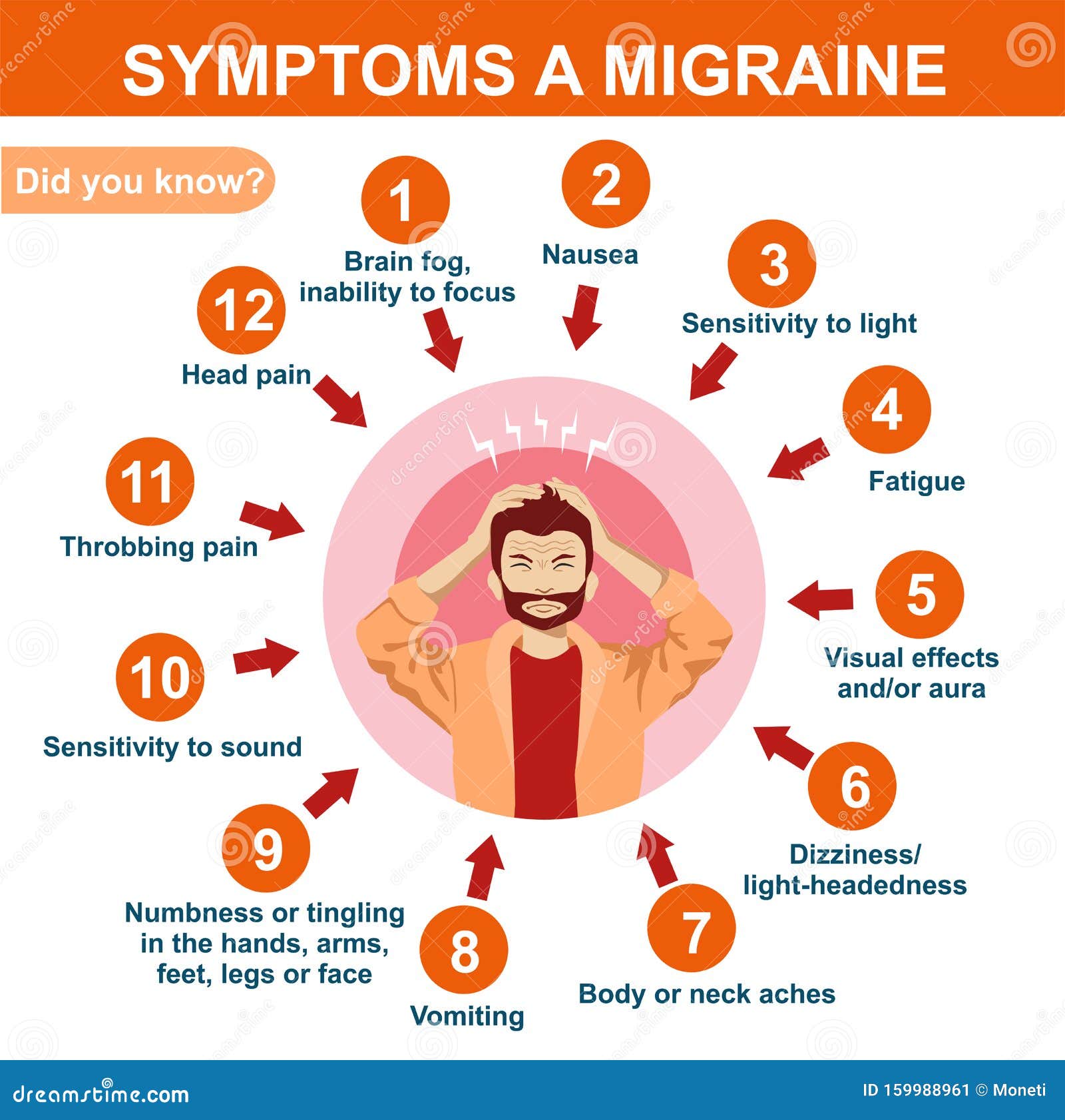
Migraines and panic attacks are distinct conditions, but they share some overlapping symptoms and triggers, leading to a higher likelihood of co-occurrence. Let’s break down what each one entails:Migraine: A migraine is a type of headache that can cause severe throbbing pain or a pulsing sensation, usually on one side of the head. It is often accompanied by nausea, vomiting, and extreme sensitivity to light and sound. Some people experience an "aura" before or during a migraine, which can include visual disturbances like flashing lights or blind spots.
Panic Attack: A panic attack is a sudden episode of intense fear that triggers severe physical reactions when there is no real danger or apparent cause. They can be incredibly frightening, making you feel like you're losing control, having a heart attack, or even dying.
Here’s a quick comparison of key symptoms:Migraine Symptoms:
Throbbing head pain (often one-sided)
Nausea and/or vomiting
Sensitivity to light, sound, and smells
Visual disturbances (aura)
Fatigue
Dizziness
Panic Attack Symptoms
Sudden overwhelming fear
Rapid heartbeat
Sweating
Trembling or shaking
Shortness of breath
Chest pain
Dizziness or lightheadedness
Numbness or tingling
Feeling of unreality or detachment
While the core experiences are different, some symptoms, like dizziness, nausea, and a feeling of being unwell, can overlap, making it hard to differentiate between them at times.
The Link Between Migraine and Panic Attacks: Is There a Connection?
Research suggests a significant association between migraines and panic disorder. People who experience migraines, particularly those with aura, are more likely to experience panic attacks and panic disorder. Several factors could explain this link: Shared Biological Pathways: Both migraines and panic attacks involve imbalances in brain chemicals, such as serotonin and norepinephrine. These neurotransmitters play a crucial role in mood regulation, pain perception, and anxiety response. Genetic Predisposition: There may be a genetic component that increases vulnerability to both conditions. If you have a family history of migraines or anxiety disorders, you may be more likely to experience them yourself. Stress and Anxiety: Chronic stress and anxiety are known triggers for both migraines and panic attacks. The stress of anticipating or experiencing a migraine can trigger a panic attack, and vice versa. Conditioning and Learned Association: Experiencing a migraine can be incredibly frightening, especially if it's severe. This fear can lead to anxiety and panic attacks, particularly if you develop a conditioned response associating certain environments or situations with migraines.
Causes and Triggers for Migraines and Panic Attacks
Identifying your specific triggers is key to managing both migraines and panic attacks. While triggers vary from person to person, some common culprits include:Migraine Triggers:
Stress: One of the most common triggers. Hormonal Changes: Fluctuations related to menstruation, pregnancy, or menopause. Dietary Factors: Aged cheeses, processed meats, chocolate, caffeine, alcohol (especially red wine), and artificial sweeteners. Sensory Stimuli: Bright lights, loud noises, strong smells. Changes in Sleep Patterns: Lack of sleep, oversleeping, or jet lag. Weather Changes: Changes in barometric pressure. Dehydration: Not drinking enough water. Skipping Meals: Low blood sugar levels.
Panic Attack Triggers
Stressful Life Events: Job loss, relationship problems, financial difficulties. Trauma: Past traumatic experiences can trigger panic attacks. Medical Conditions: Certain medical conditions, like hyperthyroidism or heart problems, can sometimes trigger panic attack symptoms. Substance Use: Withdrawal from alcohol or drugs, or even overuse of caffeine. Specific Phobias: Fear of heights, enclosed spaces, or social situations. Remembering Traumatic Events: Thinking about a particularly scary past experience can trigger an attack.
Migraines, Panic Attacks, and Hormones: Special Considerations for Women
Hormonal fluctuations play a significant role in both migraines and panic attacks, particularly for women. Menstrual migraines, for instance, are triggered by the drop in estrogen levels before menstruation. Perimenopause and menopause can also lead to increased frequency and severity of migraines and panic attacks due to fluctuating hormone levels. Discussing these hormonal influences with your doctor is essential for developing a tailored management plan.
Risks and Misconceptions
It's important to separate fact from fiction when it comes to migraines and panic attacks. Understanding the risks and misconceptions can help alleviate anxiety and promote informed decision-making.
Misconception: Migraines are "just headaches." Fact: Migraines are complex neurological conditions that involve much more than just head pain. They can significantly impact a person's quality of life and ability to function.
Misconception: Panic attacks are a sign of weakness. Fact: Panic attacks are a result of a dysregulation in the body's natural "fight-or-flight" response. They are not a reflection of personal weakness or character flaws.
Risk: Chronic migraines and panic attacks can lead to: Depression and Anxiety: The constant fear and anticipation of attacks can contribute to mood disorders. Social Isolation: People may avoid social situations due to fear of having an attack in public. Decreased Quality of Life: Both conditions can interfere with work, school, and personal relationships. Medication Overuse Headache:Overuse of pain medication for migraines can paradoxically lead to more frequent headaches.
Important Note: Panic attacks donotcause heart attacks, although the chest pain and rapid heartbeat can feel very similar. However, if you have a history of heart problems, it's always best to seek medical attention to rule out any underlying cardiac issues.
Coping and Management Strategies
Managing migraines and panic attacks often requires a multi-faceted approach that addresses both immediate symptoms and underlying causes. Here are some strategies you can use:Immediate Calming Strategies for Panic Attacks:
Deep Breathing: Practice slow, deep breathing to calm your nervous system. Try the 4-7-8 technique: inhale for 4 seconds, hold for 7 seconds, and exhale for 8 seconds. Grounding Techniques: Use your senses to anchor yourself in the present moment. Describe five things you see, four things you can touch, three things you can hear, two things you can smell, and one thing you can taste. Progressive Muscle Relaxation: Tense and release different muscle groups in your body to reduce tension. Visualization: Imagine a peaceful scene, like a beach or a forest. Focus on the details and engage all your senses. Cold Water: Splash cold water on your face or hold an ice pack to your forehead to stimulate the vagus nerve and slow down your heart rate. Mantras: Repeat a calming phrase or affirmation, such as "This will pass" or "I am safe."
Long-Term Strategies for Migraines and Panic Attacks
Therapy: Cognitive Behavioral Therapy (CBT) can help you identify and change negative thought patterns and behaviors that contribute to anxiety and migraines. Exposure therapy can be helpful if your panic attacks are triggered by specific situations. Medication:
SSRIs (Selective Serotonin Reuptake Inhibitors): Commonly used to treat anxiety and depression, and can also help reduce the frequency of panic attacks.
Beta-Blockers: Can help reduce physical symptoms of anxiety, such as rapid heartbeat and trembling.
Triptans: Effective for treating acute migraine attacks.
CGRP Inhibitors: A newer class of medications specifically designed to prevent migraines.
Anti-anxiety Medication (Benzodiazepines): While effective for immediate relief of panic attacks, these are typically prescribed with caution due to the risk of dependence. Lifestyle Changes:
Regular Sleep Schedule: Aim for 7-9 hours of quality sleep per night.
Hydration: Drink plenty of water throughout the day.
Healthy Diet: Eat regular meals and avoid trigger foods.
Exercise: Regular physical activity can reduce stress and improve mood.
Stress Management Techniques: Practice relaxation techniques, such as yoga, meditation, or tai chi.
Alternative and Supportive Practices
Meditation and Mindfulness: Can help you become more aware of your thoughts and feelings and reduce reactivity to stress. Acupuncture: Some studies suggest that acupuncture can be effective for migraine prevention and anxiety reduction. Biofeedback: A technique that teaches you how to control your body's physiological responses, such as heart rate and muscle tension. Yoga: Integrates physical postures, breathing techniques, and meditation to promote relaxation and reduce stress.
Medical & Safety Guidance: When to Seek Help
While many migraines and panic attacks can be managed with self-help strategies, it's important to know when to seek professional medical attention.
Seek Urgent Care If
You experience sudden, severe headache unlike anything you've had before.
You have neurological symptoms, such as weakness, numbness, or difficulty speaking.
You experience chest pain, shortness of breath, or loss of consciousness.
You have a fever, stiff neck, or rash along with your headache.
Talk to a Doctor If
Your migraines or panic attacks are frequent or severe and interfere with your daily life.
You have any underlying medical conditions, such as heart disease or diabetes.
You are pregnant or breastfeeding.
You have a history of trauma or abuse.
You are experiencing symptoms of depression or anxiety.
Your current treatment plan is not effective.
Your doctor can help you develop a comprehensive treatment plan that may include medication, therapy, and lifestyle changes.
FAQs About Migraines and Panic Attacks
Can a migraine trigger a panic attack?
Yes, the pain and other symptoms of a migraine can be frightening and overwhelming, which can trigger a panic attack in susceptible individuals.
How can I tell the difference between a migraine and a panic attack?
Migraines typically involve head pain, nausea, and sensitivity to light and sound, while panic attacks involve sudden, intense fear and physical symptoms like rapid heartbeat and shortness of breath. However, some symptoms can overlap, making it difficult to differentiate between the two. If you're unsure, it's best to consult with a doctor.
Are migraines and panic attacks related to anxiety?
Yes, anxiety can be a trigger for both migraines and panic attacks. Chronic anxiety can increase the frequency and severity of both conditions.
What medications can help with both migraines and panic attacks?
Some medications, such as SSRIs and beta-blockers, can be effective for both migraines and panic attacks. Your doctor can help you determine the best medication for your individual needs.
Can lifestyle changes really make a difference in managing migraines and panic attacks?
Yes! Lifestyle changes, such as regular sleep, hydration, a healthy diet, and stress management techniques, can significantly reduce the frequency and severity of both migraines and panic attacks.
Is there a cure for migraines and panic attacks?
While there is no cure for either condition, both migraines and panic attacks can be effectively managed with a combination of medication, therapy, and lifestyle changes. Many people find significant relief with a comprehensive treatment plan.
Can essential oils help with migraines or panic attacks?
Some people find that certain essential oils, such as lavender or peppermint, can help reduce anxiety and ease headache pain. While research is limited, these oils may offer a complementary approach to managing symptoms. Always use essential oils with caution and consult with a healthcare professional before using them, especially if you are pregnant or have any underlying medical conditions.
Conclusion
The connection between migraines and panic attacks can be complex and challenging, but understanding the interplay between these conditions is the first step toward finding relief. By identifying your triggers, practicing coping strategies, and seeking professional help when needed, you can effectively manage both migraines and panic attacks and improve your overall quality of life. Remember, you are not alone, and there is hope for a brighter, healthier future. If these attacks are disrupting your daily life, it's vital to consult with a healthcare professional for personalized guidance and support.
